Attitudes towards psychedelics are evolving, with growing evidence supporting their potential to treat a range of mental health conditions including anxiety, depression, post-traumatic stress disorder and addiction. In 2023, Australia became the first country in the world to approve psychedelics to treat specific mental health conditions. A handful of other countries are also moving in that direction.
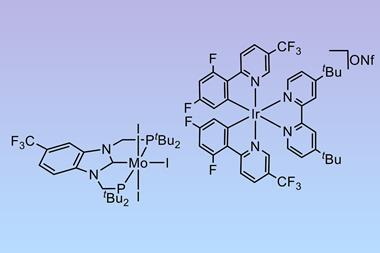
Drugs such as LSD and psilocybin stimulate neurons to grow new branches and make more synaptic connections, which is thought to be behind their long-term therapeutic effects. One of several barriers to psychedelics’ widespread clinical use is their hallucinogenic effects, so patients require close supervision and the treatment is unsuitable for those with a diagnosis that involves psychosis, like schizophrenia. Chemistry advances, however, are pushing forward research into non-hallucinogenic psychedelic analogues that could bypass these limitations.
Growing understanding of how psychedelic molecules interact with the brain is central to this progress. Classic psychedelics are understood to act as serotonin receptor agonists, particularly at the 5-hydroxytryptamine 2A (5-HT2A) receptor. But recent chemical studies have been digging deeper. An analysis of psychedelics’ electron transfer properties last year suggested that the electron-accepting capacity of these molecules correlates strongly with their potency.1 LSD, for instance, was both the most potent hallucinogen tested and the strongest electron acceptor. Moreover, research published in 2023 found that psychedelic molecules’ lipophilicity seemed to correlate with their ability to promote neuron growth.2
Such insights are supporting rational drug design, which in turn will benefit from advances in chemical synthesis. A study we covered in May, for example, saw researchers develop a 12-step synthesis to make a molecule that differs from LSD in the positioning of two atoms. JRT, as the new molecule is known, only partially actives the 5-HT2A receptor: rodent models showed it increased the density of neural branching in the prefrontal cortex but did not produce hallucinogenic-like behaviours seen with LSD. With continued innovation, skeletal editing techniques will surely come into their own here by helping to create analogues that were previously inaccessible or required lengthy syntheses.
Of course, challenges remain beyond core chemistry. Human clinical trials, including participants of both sexes, are essential since animal models can’t replicate the psychological context that shapes human experiences with psychedelics. We also need to establish whether hallucinations are necessary for psychedelics’ therapeutic effects in humans.
As we also reported on recently, new evidence suggests psychoactive plants have been used in the Peruvian Andes since the first millennium BCE. In ancient civilisations, the hallucinogenic properties of these plants played a powerful cultural role in society. In the future, psychedelics without hallucinations may play a different, but equally powerful, role in society by transforming how we treat mental health conditions.
References
1 A Martínez et al, ACS Omega, 2024, 9, 38, 39965 (DOI: 10.1021/acsomega.4c05726)
2 M V Vargas et al, Science, 2023, 379, 700 (DOI: 10.1126/science.adf0435)















No comments yet